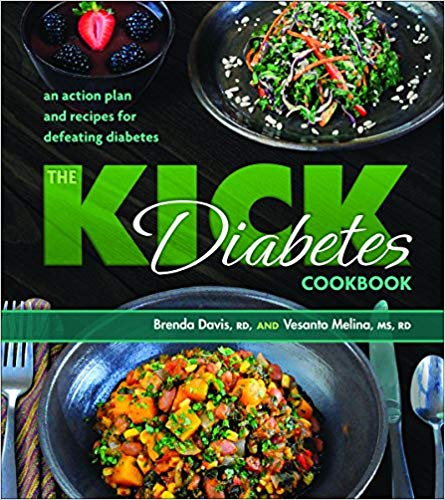
by Brenda Davis, RD and Vesanto Melina, MS, RD[br][br]
[br]
According to the Centers for Disease Control and Prevention, one in eight American adults had diabetes in 2014. If the current trends continue, they estimate that as many as 1 in 3 adults will have diabetes by 2050. The rate of diabetes has increased from 0.9 percent in the late 1950s to 9.3 percent in 2014 (12.3% in those over the age of 20 years). The figures are even more staggering among American seniors (those aged 65 years or more) – over 25% have type 2 diabetes, and over 50% have pre-diabetes. While statistically, diabetes is the 7th leading cause of death in the United States, this figure belies the fact that most people with diabetes do not die of diabetes: they die heart disease, kidney failure, and other complications. Globally, diabetes has become the 21st century plague, crippling rich and poor nations alike.
[su_spacer]
What is Diabetes?
[su_spacer]
Diabetes is a metabolic disorder that diminishes the body’s ability to usher glucose into cells so it can be used for energy. Glucose is the primary source of energy for the body, and in order for glucose to enter our cells a “gatekeeper” called insulin must let it in. People with diabetes either do not produce any insulin, do not produce enough insulin, or have become “resistant” to the insulin that they produce. This means insulin cannot do its job and blood glucose levels begin to rise. When blood glucose is elevated over time, body tissues become awash in sugar and health tumbles down a rather predictable slippery slope.
[su_spacer]
There are two main types of diabetes: type 1 and type 2. Type 1 diabetes is characterized by lack of insulin production by the pancreas, and it is generally regarded as an autoimmune disease. It occurs suddenly, and most often affects children and adolescents. Type 2 diabetes is distinguished by the preservation of insulin production, but faulty insulin action. Essentially the product of diet and lifestyle, type 2 diabetes is an insidious disease, often going undetected for many years.
Globally, type 2 diabetes accounts for over 90 percent of all diabetes cases.
The rise in diabetes runs roughly parallel that of overweight and obesity, with risk doubling in those who are overweight and tripling in those who are obese. While excess body fat plays a strong role in this disease, the way the fat is distributed is perhaps even more significant. Weight concentrated around the abdomen and in the upper part of the body (apple-shaped) increases risk far more than weight that settles around the legs and hips (pear-shaped). Fat that collects in and around vital organs (visceral fat) is far more damaging than fat that accumulates close to the skin’s surface (subcutaneous fat). Type 2 diabetes was once referred to as “adult-onset diabetes” because it was a disease rarely occurred in people under 50 years of age. Today, type 2 diabetes is seen in young adults, teens, and even children. Untreated or poorly controlled type 2 diabetes is a leading cause of blindness, premature heart attack and stroke, kidney failure, nerve damage, and amputations.
[su_spacer]
Diabetes is defined as fasting blood glucose of at least 126 mg/dl (7.0 mmol/L), while pre-diabetes occurs when blood glucose reaches at least 110 mg/dl (6.1 mmol/L). Pre-diabetes is often manifested as “metabolic syndrome”, a cluster of risk factors characterized by elevated blood glucose, abdominal obesity, elevated blood pressure, elevated triglycerides, and low HDL-cholesterol levels. A cascade of problems ensues that commonly results in full-blown type 2 diabetes.
[su_spacer]
The Luck of the Draw?
[su_spacer]
Some people believe that type 2 diabetes is more a matter of bad genes than bad habits. While it is true that some populations have a greater susceptibility to the disease, genes serve primarily as a loaded gun; it is almost always diet and lifestyle that pull the trigger.
[su_spacer]

[su_spacer]
In a laudable effort to reverse the Marshallese diabetes epidemic, Canvasback Missions Inc. (a Christian, non-profit organization, specializing in medical missions to remote South Pacific islands), in partnership with Loma Linda University and the Marshall Islands Ministry of Health, launched a lifestyle-based diabetes research study in 2006. I was hired to serve as lead dietitian; to design and implement the diet portion of the treatment program. For each intervention, approximately half of the qualified participants were assigned to an intervention group and half to a control group. Intervention participants received diet and lifestyle instruction over a 3-6 month period, while the control group received the “usual care” (advice from a physician and/or other health care worker to exercise, eat more healthfully and take the appropriate medication). Control group participants were guaranteed a place in the intervention group once their six-month control period had been completed (although their data could not used be used in the analysis). The two key elements of the lifestyle intervention were diet and exercise. The primary objective of treatment was to overcome insulin resistance and to restore insulin sensitivity as much as was physiologically possible. The diet was designed to support blood glucose control, reduce inflammation, reduce oxidative stress and restore nutritional status. To accomplish this task, the dietary parameters were set as follows:
[su_spacer]
-
- Whole foods, plant-based diet
- Generous servings of non-starchy vegetables and legumes
- Controlled portions of intact (whole) grains, starchy vegetables, nuts and seeds
- Minimal refined carbohydrates
- Minimal ground flaked and puffed grains
- Very high fiber (40-50+ grams per day)
- High viscous fiber foods (flax, oats, barley, beans, guar gum, psyllium)
- Moderate fat from healthful sources such as nuts and seeds (15-25% fat)
- Low saturated fat (<5-6% of calories)
- Zero trans fatty acids
- Sufficient omega-3 fatty acids
- High phytochemical and antioxidant foods
- Low dietary oxidants
- Low glycemic load
- Moderate- sodium (Less than 2300 mg/day)(We now recommend <1500 mg/day)
[su_spacer]
[su_spacer]
Could It Work at Home?
[su_spacer]
Some people ask if the kind of program we use in the Marshall Islands could work in North America and other developed parts of the world. If the impoverished people of the Marshall Islands can succeed with the enormous barriers they face, it should be a relative breeze at home. The Marshallese have put together low cost, healthful meals despite the high cost and poor quality of their produce, their infertile soils, and their lack of resources. They have managed with little education and marginal English skills. They have succeeded with few gyms, no hiking trails, and a cultural taboo against women wearing pants, shorts or other fitness wear. Their example inspires hope for everyone, everywhere.
References
Salas-Salvadó J, Martinez-González MÁ, Bulló M, Ros E. The role of diet in the prevention of type 2 diabetes. Nutr Metab Cardiovasc Dis. 2011 Sep;21 Suppl
2:B32-48.
Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: US Department of Health and Human Services; 2014.
Centers for Disease Control and Prevention. Diabetes Report Card 2012. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2012.
[su_divider]
 Every day, and in countries around the world, more and more people are turning to a plant-based diet for reasons of personal health, environmental concerns, and to cultivate a compassionate lifestyle. The ‘seeds’ of this plant-based movement started sprouting years ago with visionary leaders that include Brenda Davis, RD and Vesanto Melina MS, RD. They have been steadily educating professionals, governments and ‘heads of state’ on the numerous benefits of a plant-based diet, creating ripples of awareness and change. We’re fortunate to have these two dynamos on our faculty and offering their research-based curriculum for an Advanced Vegan and Raw Food Nutrition Educator Certification program at Living Light.
Every day, and in countries around the world, more and more people are turning to a plant-based diet for reasons of personal health, environmental concerns, and to cultivate a compassionate lifestyle. The ‘seeds’ of this plant-based movement started sprouting years ago with visionary leaders that include Brenda Davis, RD and Vesanto Melina MS, RD. They have been steadily educating professionals, governments and ‘heads of state’ on the numerous benefits of a plant-based diet, creating ripples of awareness and change. We’re fortunate to have these two dynamos on our faculty and offering their research-based curriculum for an Advanced Vegan and Raw Food Nutrition Educator Certification program at Living Light.







